One often hears alphabets like ‘A’, ‘B’, and sometimes ‘O’, in response to queries regarding someone’s blood type. These alphabets merely denote the presence of certain antigens which categorizes blood into specific types. This concept of classifying blood groups according to the presence or absence of antigens A and B is known as the ABO blood group system. It is the first-ever blood group system to be discovered.
Before its discovery, people assumed the blood in every individual was the same. This discovery proved a tremendous boon, giving way to safe blood transfusion, the study of inheritance, and paternity testing, and providing further insight into the study of different populations.
History: An Austrian scientist, Karl Landsteiner discovered two kinds of agglutinogens or antigens i.e. A and B antigens from the surface of RBCs in humans in 1900. He noted that serum from some individuals agglutinated the RBCs from other individuals. He explained this phenomenon as a reaction between antibodies present in serum and antigens on the RBCs. A conclusion was reached that a person may either have one of the A or B antigens or may not have both of them. Primarily, he suggested the presence of 3 types of blood groups; Type A, Type B, and Type O giving rise to the concept of the ABO blood group system. He won a Nobel prize for this discovery.1
Later in 1902, his students, Van Decastello and Sturli discovered the AB blood group, having both A and B antigens. In 1910, it was proved that RBC antigens are inheritable and there exists a sort of codominance between A and B antigens.
Formation of ABO antigen and antibody: Antigens of ABO blood group are mucopolysaccharides (sugars + amino acids) of 300,000 molecular weight. They are found in attachment with various components in the cell membrane of RBCs. A person’s DNA plays a role in enzymes present in their body which in turn catalyzes various reactions that form the blood group antigens.
ABO antibodies are formed in the serum naturally. However, the original mechanism behind the synthesis of these natural antibodies is not exactly known. A popular hypothesis suggests that the antibodies synthesis is stimulated when the immune system encounters the missing ABO blood group antigens through food or microorganisms.2
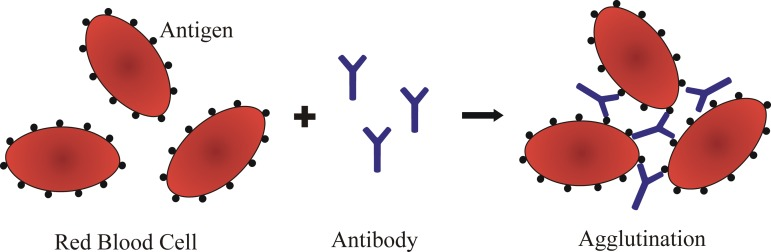
Blood Agglutination: The body’s immune system produces antibodies in serum against antigens that are absent in the RBCs of the individual. For instance, A person with blood group A contains antibodies against B antigen and vice versa. For a person with the AB blood group, no antibodies are formed and for the O blood group antibodies against both antigens A and B are present.
Antibodies randomly bind to opposing antigen surfaces. It causes clumping and the phenomenon is called agglutination. The four blood types have different agglutinizing properties.3 This fact plays a vital role during blood transfusion. Blood transfusion can only occur between individuals if the donor’s antigens do not trigger an immune response by the receiver’s antibodies. The type of blood transfusion possible can be summarized in the following table.
| Blood group | Antigen(s) present on RBCs | Antibodies present in serum | Can give blood to group | Can receive blood from group |
| A | A antigen | Anti-B | A, AB | O, A |
| B | B antigen | Anti-A | B, AB | O, B |
| AB | A antigen and B antigen | None | AB | AB, A, B, O |
| O | None | Anti-A and Anti-B | AB, A, B, O | O |
Blood transfusion between mismatched groups (For example A to B) may trigger the receiver’s immune system to attack the donated blood cells and destroy them i.e. acute immune hemolytic reaction. It occurs within 24 hours of transfusion. Clumping of the RBCs may occur which causes blood clots in capillaries, depriving vital organs of normal blood supply which may lead to death.
The risk of fatality due to ABO mismatched red blood cell transfusion is estimated to be 1 to 4 per 10,000,000 of each RBC unit transfused.4 Hence, blood product safety has been an area of priority all over the world. WHO has been the leading figure in pushing forward this agenda worldwide. According to its survey conducted in 2018, 113 out of 171 reporting countries have specific legislation regarding the safety and quality of blood transfusion.5
References:
- Dr. P.S. Verma, Dr. C.K. Agrawal. Cell Biology, Genetics, Molecular Biology, Evolution and Ecology. fourteenth. (Bharatnagar S, Pradhan S, eds.). S.CHAND & COMPANY PVT.LTD.; 2016.
- L D, Bethesda. Blood Groups and Red Cell Antigens. National Center for Biotechnology(U.S.); 2005.
- Clark MA, Choi J, Douglas M. Biology 2e. Second. The Rice University Press; 2020.
- Uramatsu M, Maeda H, Mishima S. Serious hazards of transfusion: evaluating the dangers of a wrong patient autologous salvaged blood in cardiac surgery. Cardiothoracic Surgery. Published online 2022.
- https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability
- Parslow TG, Stites DP, Terr AI, Imboden JB.Imunologia Médica. 10th ed Rio de Janeiro: Guanabara Koogan, 2004.
Major blood banks in and around Kathmandu Valley
Bhaktapur NRCS Blood Bank,
Bhaktapur
01-6611661, 01-6612266
Central NRCS Blood Bank,
Soaltee-Mode
01- 4288485
Kantipur Hospital Pvt. Ltd.
Subidhanagar Tinkune, Kathmandu, Nepal
01-4111692
Lalitpur NRCS Blood Bank,
Pulchowk
+97715427033
Frontline Hospital Blood Bank,
Old Baneshwor , Kathmandu
01-5970132
Teaching Hospital,
Maharajgunj, Kathmandu
01-4412303, 01-4410911
Gangalal Hospital,
Bansbari, Kathmandu
01-4371322
Himal Hospital,
Gyaneshwor, Kathmandu
986-2737316
Grande Hospital,
Dhapasi
01-5159266
Prasuti Griha,
Thapathali, Kathmandu
01-4260405
Nepal Mediciti Hospital,
Nakhkhu Ukalo, Lalitpur
01-4217766
Bir Hospital,
New road gate, Kathmandu
01-4221119, 01-4221988
Nepal Police Hospital,
Maharajgunj, Kathmandu
01-4412430
Civil Hospital,
Minbhawan, Kathmandu
01-4107000
Patan Hospital,
Patan, Lalitpur,
01-5522295
Birendra Army Hospital,
Kathmandu
01-4271941
Nepal Medical College,
Gokarneswor, Kathmandu
01-4911008
Kathmandu Medical College And Teaching Hospital,
Sinamangal, Kathmandu
01-4469064
Major blood banks outside Kathmandu Valley
NRCS Regional BTSC,
Banke, Nepalgunj
081 – 520174
NRCS Regional BTSC,
Bharatpur, Chitwan
056 – 520880
NRCS Regional BTSC,
Pokhara, Kaski
061 – 521091, 061 – 540191
NRCS Regional BTSC,
Rangeli Road, Biratnagar
021 – 523326
Dhulikhel Hospital,
Dhulikhel
011 – 490497
Manipal Teaching Hospital,
Pokhara, Kaski
061-526416
BP Koirala Memorial Cancer Hospital,
Bharatpur
056-524501
Janaki Medical College Teaching Hospital,
Dhanusha, Janakpur
01-4435957
Universal College of Medical Sciences,
Bhairahawa, Sidarthnagar
071-522896
Bardiya DBTSC,
Bardiya
084‐420835
Dang District BTSC,
Ghorahi, Dang
082‐561460
Jumla District BTSC,
Jumla
087‐520036
Sunsari District BTSC,
Dharan
025 – 525555
Jhapa District BTSC,
Birtamode, Jhapa
023‐541833
Ilam District BTSC,
Ilam
027‐520022
Panchthar District BTSC,
Panchthar
024‐570273
Butwal District BTSC,
Butwal
071‐550462
Siraha District BTSC,
Siraha
033‐560975
Terhathum District BTSC ,
Myaglung
026‐460101
Makawanpur District BTSC,
Makwanpur
057‐522977
Parsa District BTSC,
Parsa
051 – 522504
Dhanusha District BTSC,
Janakpur Provincial Hospital
041 – 520870
Kavre District BTSC,
Banepa, Kavre
011 – 661431
Kanchanpur District BTSC,
Kanchapur
099‐525588
Scheer Memorial Hospital,
Banepa, Kavre
011 – 661111
Nepalgunj Medical College,
Banke
972 – 3001626
Tikapur Hospital,
Kailali
091-560406
Padama Hospital,
Kailali
099-550355
United Mission Hospital,
Palpa
075 – 520958
Lamjung Community Hospital,
Besisahar, Lamjung
066 – 520183
Dr. Megh Bahadur Parajuli Community Hospital,
Illam
027-520417
Relevant Links:






Pingback: Apoptosis: Significance, Mechanism and Regulation - Aneknowledge.com